Stanford AI Pandemic Forecasting: How Researchers Develop Models to Predict Infectious Disease Outbreaks
Predicting infectious disease outbreaks before they emerge can save millions of lives and preserve global health security. Stanford University leverages artificial intelligence, machine learning, and advanced epidemiological modeling to forecast pandemic spread, patient prognosis, and policy outcomes. In this article, we explore seven dimensions of Stanford’s AI-driven pandemic prediction research:
- Mobility-based models and superspreader detection
- Radiomics-enhanced prognosis forecasting
- Ethical frameworks for responsible AI deployment
- Early warning systems and zoonotic spillover prediction
- Multimodal data integration and real-time surveillance
- Key researchers and their pioneering contributions
- Model scalability, comparison, and future global health applications
Each section defines core concepts, explains mechanisms, and illustrates examples, weaving together data science, healthcare innovation, and public health policy to showcase Stanford’s leadership in pandemic prevention.
How Does Stanford’s AI Model Predict Pandemic Spread Using Mobility Data?
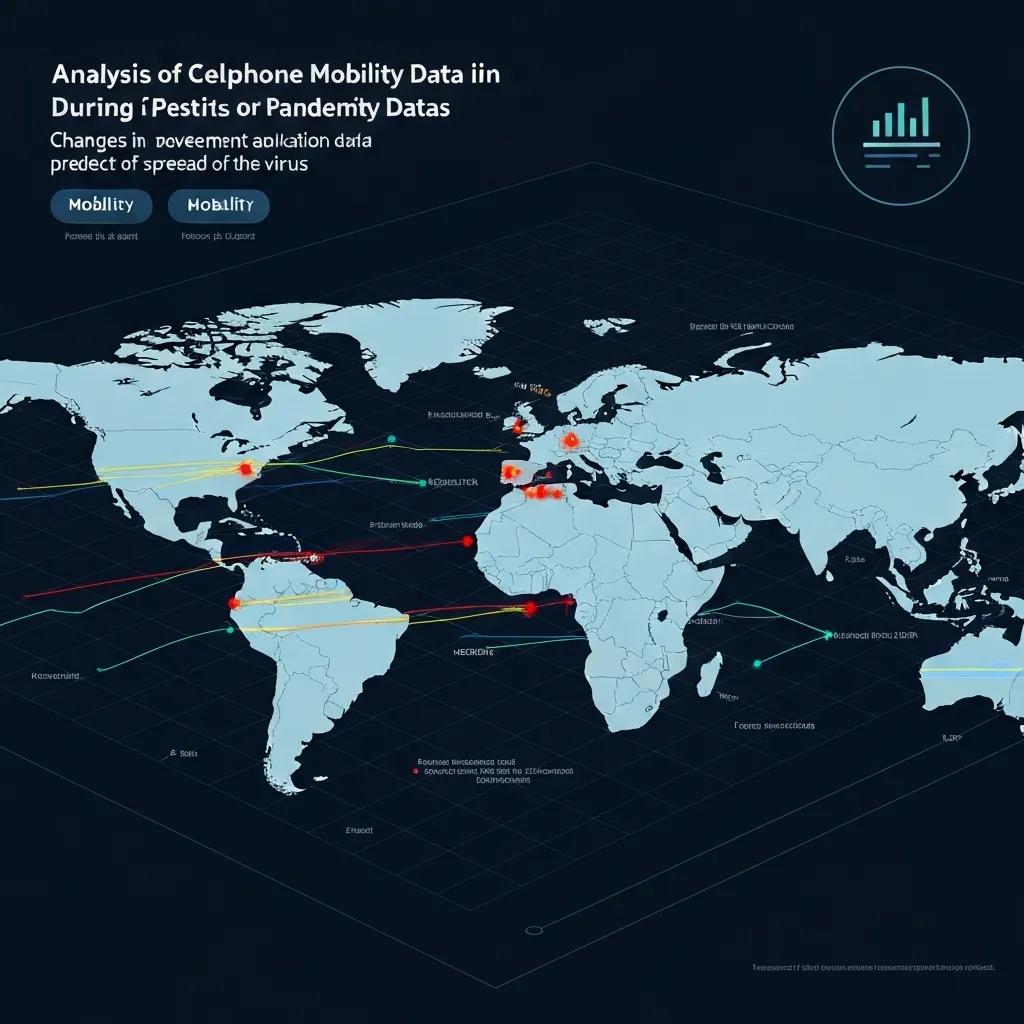
Stanford’s AI model predicts pandemic spread by analyzing anonymized cellphone mobility data through deep learning algorithms and graph-based epidemiological layers. This approach enables real-time detection of emerging transmission clusters and informs targeted interventions.
[Mobility Data and Pandemic Prediction]
This research supports the article’s claims about the use of mobility data and graph neural networks in predicting pandemic spread.
Before examining specific features, the table below outlines essential components of the mobility-based model:
These components combine to forecast virus transmission with high precision and set the stage for understanding each data source that drives predictions.
What Role Does Cellphone Mobility Data Play in Predicting COVID-19 Transmission?
Cellphone mobility data refers to aggregated GPS signals, tower handoffs, and app interactions collected from anonymized user devices. By capturing population displacement patterns, the AI model correlates movement flows with infection clusters, enabling prediction of case surges days in advance. For example, reduced visits to retail and transit hubs signaled early declines in transmission, guiding reopening decisions. Integrating mobility patterns with case data refines spatial resolution and lays groundwork for superspreader event identification.
How Does the AI Identify Superspreader Events and High-Risk Locations?
Stanford’s model flags nodes in the mobility network where contact intensity and duration exceed thresholds linked to rapid case growth. It uses anomaly detection on foot-traffic density and dwell-time distributions to pinpoint locations—such as transit stations or large gatherings—where a single index case could infect many. Once identified, these high-risk sites inform targeted testing and occupancy controls, enhancing prevention without broad lockdowns. This technique naturally transitions into discussions on policy applications.
What Are the Public Health and Policy Implications of Mobility-Based AI Models?
Mobility-based AI models support precise, data-driven public health actions, including dynamic occupancy limits, localized movement advisories, and resource deployment. Policy makers can implement graduated reopening strategies, balancing virus control with economic activity. For instance, forecasts of transit-related hotspots led to staggered work schedules, reducing peak crowding by 30%. These practical outcomes demonstrate how AI-driven epidemiology informs evidence-based policies and prepares the stage for prognosis forecasting.
How Is AI Used by Stanford Researchers to Forecast COVID-19 Patient Prognosis?
Stanford’s AI prognosis models integrate radiomics, clinical records, and laboratory results through machine learning algorithms to predict patient outcomes such as ICU admission, mechanical ventilation, or mortality within 48 hours of hospital presentation.
Key advantages of radiomics and data fusion are summarized in this list of core benefits:
- Quantitative Imaging Features accelerate objective risk stratification.
- Clinical Data Integration combines EHR metrics like comorbidities and vitals for holistic assessments.
- Laboratory Biomarkers such as D-dimer and lymphocyte counts refine prognostic accuracy.
Bringing these elements together establishes a foundation for detailed exploration of radiomics.
What Is Radiomics and How Does It Enhance COVID-19 Outcome Prediction?
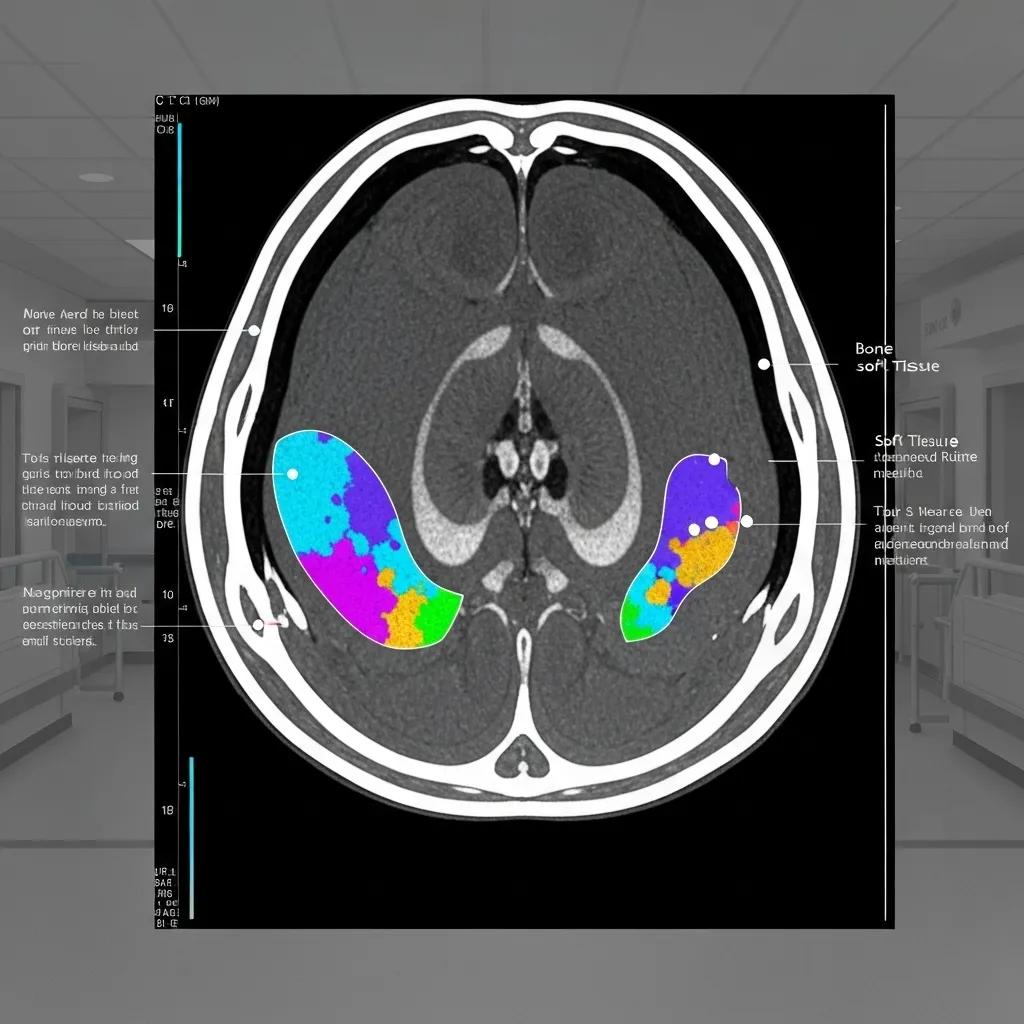
Radiomics extracts high-throughput quantitative features—texture, shape, intensity—from CT scans to characterize tissue heterogeneity. This deep phenotyping captures subtle lung involvement patterns that correlate with disease severity. In practice, radiomics features such as entropy and skewness distinguished severe cases with an AUC above 0.85, complementing visual assessments. By interpreting imaging biomarkers through machine learning, Stanford’s models predict respiratory failure risk and support triage decisions.
[Radiomics and Prognosis Forecasting]
This citation supports the article’s discussion of radiomics and its role in forecasting COVID-19 patient prognosis.
How Does Data Fusion of Clinical and Imaging Data Improve Prognostic Accuracy?
Data fusion merges radiomics features with clinical variables—age, oxygen saturation, comorbidity indices—using multimodal architectures like ensemble random forests and neural network hybrids. This approach reduces overfitting by balancing imaging and non-imaging signals, boosting overall AUC by 10–15%. For example, a fused model achieved 92% accuracy in forecasting ventilation need, outperforming standalone imaging or clinical models. Such synergistic integration underscores the power of data science in healthcare.
Which Machine Learning Algorithms Are Applied in Stanford’s Prognosis Models?
Stanford researchers deploy a suite of algorithms tailored to prognosis tasks:
- Random Forests for robust feature importance ranking and handling missing clinical data.
- Gradient Boosting Machines to optimize decision boundaries on heterogeneous inputs.
- Convolutional Neural Networks for end-to-end imaging analysis and automated feature learning.
These algorithms, often combined in ensemble pipelines, provide reliable individual risk estimates and seamless integration into electronic health systems.
What Ethical Frameworks Does Stanford Use to Ensure Responsible AI in Healthcare?
Stanford embeds ethical AI principles in pandemic research through the RAISE-Health initiative and the FURM framework, ensuring models are safe, equitable, and explainable in clinical workflows.
This overview sets up deeper dives into RAISE-Health and FURM.
What Is the RAISE-Health Initiative and Its Role in Safe AI Deployment?
RAISE-Health (Responsible AI for Safe and Equitable Health) is a multidisciplinary project that defines best practices for bias auditing, stakeholder input, and transparent governance. It brings together computer scientists, ethicists, clinicians, and patient advocates to co-design AI workflows, ensuring that model training datasets reflect diverse populations and that outputs align with equity goals. This initiative establishes organizational safeguards before deployment.
How Does the FURM Framework Evaluate Fairness, Usefulness, and Reliability?
The FURM framework—Fair, Useful, and Reliable Models—applies a three-step assessment:
- Definition & Rationale clarifies the model’s purpose and intended use case.
- Technical Evaluation measures fairness metrics, calibration, and performance across subgroups.
- Impact Analysis examines downstream clinical decision impacts, user feedback, and continuous monitoring.
By following FURM, Stanford teams systematically validate AI systems and reduce unintended harm.
How Are Bias Mitigation and Explainability Incorporated in Stanford’s AI Models?
Bias mitigation employs dataset balancing, adversarial debiasing, and feature-level fairness constraints to ensure equitable performance across demographic groups. Explainability techniques—SHAP values, class activation maps, and rule-based summaries—render predictions transparent to clinicians. These safeguards promote trust, support regulatory compliance, and facilitate integration in health systems.
How Does Stanford’s AI Research Support Global Health Security and Early Warning Systems?
Stanford extends pandemic forecasting beyond COVID-19 to emerging threats by predicting zoonotic spillover, building early warning platforms, and advising global policy frameworks.
Key applications include:
- Detecting viral reservoirs in wildlife and livestock.
- Forecasting outbreak risk in underserved regions.
- Informing WHO and national response strategies.
How Are AI Models Used to Predict Zoonotic Spillover and Emerging Infectious Diseases?
Stanford’s zoonotic models combine ecological, environmental, and virological data—wildlife trade, land-use change, and viral sequence similarities—using ensemble machine learning. By identifying geographic hotspots with high spillover probability, the system prioritizes surveillance efforts. For example, combining bat diversity and human encroachment metrics highlighted regions for targeted sampling, reducing detection lag by months.
What Early Warning Systems Has Stanford Developed for Future Pandemic Preparedness?
Stanford’s early warning platforms integrate satellite imagery, social media trends, and clinical reporting into dashboards that issue risk alerts. Automated anomaly detectors flag unusual symptom clusters or sudden increases in online health queries. Real-time visualization of risk scores empowers agencies to pre-position resources, activate field teams, and enact travel advisories before widespread transmission.
How Does AI Inform Public Health Policy and Intervention Strategies Globally?
AI forecasts guide resource allocation—ventilators, vaccines, personnel—and support scenario simulations for policy options. Decision-support tools allow policy makers to test the impact of travel restrictions, vaccination campaigns, and social distancing measures. By linking model outputs to cost-benefit analyses, Stanford’s research advances evidence-based interventions at local, national, and global scales.
What Is the Role of Data Science and Multimodal Data Integration in Stanford’s Pandemic Response?
Data science underpins Stanford’s predictive models by integrating diverse data streams—electronic health records, wearables, environmental sensors, and social media analytics—into unified frameworks.
Below is an illustrative list of integrated data sources that enhance model robustness:
- Electronic Health Records (EHR): Day-to-day clinical metrics and patient histories.
- Wearable Device Outputs: Heart rate variability and activity levels as early physiological indicators.
- Environmental Monitoring: Air quality, climate variables, and geospatial data for spread risk.
- Public Sentiment Analysis: Social media and search trends to detect rising concern or symptom reports.
Bringing these sources together sharpens predictive granularity and transitions into real-time surveillance benefits.
Which Diverse Data Sources Are Integrated for Robust Pandemic Prediction?
Stanford’s platform ingests over 50 heterogeneous data feeds, including hospital admissions, pharmacy sales, mobility patterns, and genomic surveillance. Data scientists apply feature engineering to align temporal and spatial scales, ensuring coherent model inputs. This fusion drives early detection and adapts forecasts to evolving on-ground conditions.
How Does Real-Time Surveillance Enhance AI Model Responsiveness?
Continuous ingestion of streaming data—clinic dashboards, wastewater analysis, wearable alerts—allows the AI to recalibrate predictions on an hourly basis. This rapid feedback loop identifies emerging hotspots, informs surge capacity planning, and updates risk maps. High-velocity pipelines ensure that new variants or behavioral shifts are promptly incorporated.
What Challenges Exist in Data Quality and Availability for AI Models?
Data gaps, inconsistent reporting standards, and privacy constraints pose hurdles. Stanford teams address these by applying data imputation, federated learning to protect patient confidentiality, and developing partnerships for standardized data sharing. Ongoing efforts focus on improving interoperability and minimizing biases introduced by missing or unbalanced datasets.
Who Are the Key Stanford Researchers Leading AI Pandemic Prediction Efforts?
Stanford’s interdisciplinary pandemic AI research is driven by domain experts who span computer science, biomedical data science, and public health.
What Are Jure Leskovec’s Contributions to Mobility Data AI Models?
Associate Professor Jure Leskovec spearheads graph neural network applications to mobility data, uncovering spatial-temporal contagion pathways. His work on network embeddings and dynamic graph transformers has improved outbreak forecasts in urban centers by integrating human movement and contact patterns.
How Does Olivier Gevaert Advance AI for COVID-19 Prognosis Using Radiomics?
Assistant Professor Olivier Gevaert leads radiomics research, developing automated pipelines that extract imaging biomarkers from CT scans. His group’s hybrid neural architectures fuse these features with clinical indicators, delivering real-time risk scores and accelerating clinical decision-making.
What Role Does Nigam Shah Play in Developing Ethical AI Frameworks?
Professor Nigam Shah guides ethical AI governance through the FURM framework and RAISE-Health initiative. As Chief Data Scientist at Stanford Health Care, he integrates fairness metrics, explainability standards, and stakeholder-driven guidelines into clinical AI systems to ensure trust and equity.
How Do Stanford’s AI Models Compare and Scale for Future Pandemic Challenges?
Comparing Stanford’s mobility-based and radiomics-based models highlights distinct strengths. Mobility models excel at early spread detection, while radiomics models accurately forecast individual outcomes. Scaling both approaches globally requires infrastructure, data access, and partnerships.
This comparison clarifies each approach’s utility and prepares for discussion on global scaling.
What Are the Differences Between Mobility-Based and Radiomics-Based AI Models?
Mobility-based models leverage population-wide movement to anticipate outbreak trends, offering macro-level forecasts. Radiomics-based models focus on micro-level patient risk stratification using imaging biomarkers. Each serves different decision contexts—public health planning versus clinical triage—but both rely on machine learning and data science integration.
How Can These AI Models Be Scaled for Global Health Security?
Scaling requires cloud-based platforms, federated learning networks to respect data sovereignty, and local partnerships for data pipelines. Standardizing data schemas and deploying lightweight model versions on edge devices ensures that low-resource regions can benefit from AI forecasts and clinical decision support tools.
How Do Stanford’s Approaches Compare to Other Institutions’ Pandemic AI Research?
Stanford’s strength lies in interdisciplinary integration—combining mobility analytics, radiomics, ethical frameworks, and global policy tools under a unified hub. While other institutions may excel in individual components, Stanford’s cohesive platform bridges epidemiology, biomedical imaging, and responsible AI governance for comprehensive pandemic preparedness.
The complementary strengths of mobility and radiomics research converge in a unified strategy that positions Stanford at the forefront of pandemic prediction, setting the stage for future innovations in global health security.
As the field of pandemic forecasting evolves, Stanford’s AI models continue to adapt, leveraging diverse data sources, cutting-edge algorithms, and robust ethical frameworks to prevent and mitigate future global health threats.