Football Player Kidney Injury Update: Justin Landes’s Recovery and Return to Play
Justin Landes, a standout for Lake High School’s Lake Blue Streaks, suffered a kidney injury during a recent Cleveland-area football game and is now in recovery under medical supervision. This article explains what happened, how kidney injuries present in contact sports, the diagnostic and treatment pathways clinicians use, and realistic timelines for recovery and return to play. Readers will learn the signs that require emergency care, the tests that confirm renal trauma, conservative and operative treatment options, and staged rehabilitation steps that combine physical and mental–health support. The piece also outlines prevention strategies—from protective gear to coaching technique—and details how local communities typically rally around injured athletes. Throughout, we integrate timely reporting context and expert-informed guidance so families, coaches, and athletes understand both the immediate incident and the longer medical pathway. Expect clear checklists for return-to-play, practical prevention tips for contact sports, and structured comparison tables mapping injury severity to likely recovery durations and diagnostic tests.
ARY News provides continuous regional coverage of local sports and medical updates; our editorial approach here reflects that mission. To provide timely and comprehensive news and current affairs coverage, keeping the audience informed and engaged with diverse content. As an information hub focused on accurate, current reporting, ARY News will continue following this story through verified updates and sports-safety reporting. This article follows that intent while prioritizing medical accuracy and community context. The next section narrates the incident timeline and immediate on-field response to clarify exactly how this injury unfolded.
What Happened to Justin Landes During the Football Game?
A clear incident timeline establishes how the kidney injury occurred and why immediate response matters. During the play that led to the injury, Justin sustained blunt force to the flank region after a heavy tackle, creating the mechanical conditions that can produce renal trauma in contact sports. Blunt impact transmits force to the abdomen and flank, potentially causing contusion or laceration of renal tissue and perirenal bleeding, which explains the urgent medical attention he received. Understanding the play sequence helps coaches and trainers recognize patterns of risk and refine sideline protocols that reduce time to treatment. The following subsections describe the mechanics of the injury and the on-field to emergency-room sequence that followed, which in turn informs diagnostic priorities.
How Did the Kidney Injury Occur in the Football Match?
The injury occurred when a forceful tackle landed on the player’s lower ribcage and flank, producing blunt abdominal trauma to the kidney-bearing region. Blunt impact to the flank concentrates force over the renal capsule and parenchyma, and that energy can create contusion or laceration depending on intensity and point of contact. In high-school football, lateral hits and falls onto fixed objects or turf can magnify torque and increase risk to internal organs, including the kidneys. Recognizing that mechanism clarifies why flank tenderness, referred abdominal pain, or visible bruising after such impacts warrants immediate evaluation and imaging.
What Immediate Medical Actions Were Taken After the Injury?
On-field responders first stabilized airway, breathing, and circulation and assessed for signs of shock or active bleeding before arranging rapid transfer to emergency care. Athletic trainers typically immobilize the athlete, control external bleeding if present, and monitor vitals while coordinating ambulance transport to a hospital equipped for trauma evaluation. At the emergency department, clinicians prioritize rapid assessment for hemodynamic stability, administer IV fluids if indicated, and initiate diagnostic testing such as urinalysis and imaging to evaluate for renal injury. Quick triage and transport reduce the risk of delayed diagnosis and allow timely decisions about observation, imaging, or surgery.
What Are the Symptoms and Types of Kidney Injuries in Football Players?

Kidney injuries in contact sports range from minor contusions to major lacerations, and they present with a predictable symptom set that helps clinicians triage severity. A renal contusion is a bruise to kidney tissue with intact capsule, while a laceration involves a tear to renal parenchyma and can bleed into the perirenal space; severity is commonly graded I–V in trauma scoring. Early recognition of symptoms—including blood in urine, flank pain, nausea, and dizziness—prompts timely testing and reduces risk of complications. The next subsections list common symptoms and contrast lacerations with other renal trauma subtypes to guide early decisions about diagnostics and management.
Kidney injuries present several common symptoms that are easy for parents, coaches, and trainers to watch for after an impact.
- Visible or microscopic blood in urine (hematuria): Often the earliest sign of renal trauma.
- Flank or lower back pain: Localized tenderness on the side of the injury that worsens with movement.
- Nausea, abdominal pain, lightheadedness: May indicate internal bleeding or referred pain.
- Bruising or swelling in the flank: External evidence many athletes show after blunt trauma.
These symptoms form a practical checklist for sideline evaluation and justify urgent transport when present, setting up the need for targeted diagnostic testing described next.
The evaluation of renal trauma in athletes involves a systematic approach to diagnosis and management, often guided by established grading scales.
Evaluation, Management, and Return to Play for Renal Trauma in Athletes
Renal trauma: evaluation, management, and return to play. Kidney injuries occur as a result of blunt abdominal trauma, flank trauma, or penetrating injury. With a CT scan, most institutions will use a three-phase protocol, as it allows for the most comprehensive evaluation of renal trauma.
Renal trauma: evaluation, management, and return to play, 2009
How Do Kidney Lacerations Differ from Other Renal Injuries?
Kidney lacerations involve an actual tear of renal tissue and often carry higher risk of bleeding and functional impairment than contusions, which are localized bruises without structural disruption. Vascular injuries can cause rapid blood loss and hemodynamic instability, while ureteral injuries are rarer and present with urine leakage or flank swelling without immediate hematuria. The distinction matters because lacerations, especially higher-grade tears, more often require imaging follow-up, possible embolization, or surgical repair, whereas low-grade contusions frequently respond to conservative management. Understanding these differences informs monitoring intensity, imaging choice, and the likely rehabilitation pathway.
How Is a Kidney Injury Diagnosed and Treated in Athletes?
Diagnosis and treatment follow a clear clinical pathway that balances rapid detection against avoiding unnecessary interventions. Initial bedside assessments include focused physical exam, vitals, and urinalysis to detect hematuria; imaging decisions depend on stability, with CT abdomen/pelvis with contrast serving as the diagnostic gold standard for detecting lacerations and active bleeding. Treatment choices pivot on hemodynamic status and injury grade: stable patients with minor injuries often undergo conservative management with observation and serial labs, while unstable patients or those with expanding hematoma may require angiographic embolization or surgical repair. The table below compares common diagnostic tests and their roles to clarify how clinicians select evaluations in practice.
Computed tomography (CT) scans are a cornerstone in the diagnosis and management of renal trauma, providing detailed anatomical information.
Renal Trauma Imaging: Diagnosis and Management with CT Scans
The purpose of this review is to illustrate and discuss the spectrum of imaging findings, particularly computed tomography (CT), of blunt and penetrating renal trauma, based on our own materials, according to the American Association for Surgery of Trauma (AAST) renal injury grading scale. The article also indicates the conditions in which interventional radiology procedures can be applied for the management of renal trauma.
Renal trauma imaging: Diagnosis and management. A pictorial review, 2013
What Medical Tests Confirm a Kidney Laceration?
Confirmation typically relies on CT abdomen/pelvis with intravenous contrast because it visualizes parenchymal tears, perirenal hematoma size, and active extravasation. Urinalysis, while informative for hematuria, cannot localize the injury or grade severity; bedside ultrasound (FAST) helps detect free fluid and guides emergent decisions in unstable patients. Serial laboratory tests—including hemoglobin/hematocrit—track ongoing blood loss and help determine the need for transfusion or operative intervention. Together these tests form a stepwise diagnostic pathway: bedside screening → laboratory monitoring → definitive CT when stability allows.
Various imaging modalities are available for assessing the grade of renal injury, each with its own strengths and weaknesses.
Imaging Modalities for Renal Injury Classification and Assessment
Renal injuries are classified, based on the American Association for the Surgery of Trauma classification, in to five grades of injury. Several imaging modalities have been available for assessing the grade of renal injury, each with their usefulness and limitations. Currently, plain radiographs and intravenous urography have no role in the evaluation of patients with suspected renal injury. Ultrasonography (USG) has a limited role in evaluating patients with suspected retroperitoneal injury; however, it plays an important role during follow up in patients with urinoma formation.
Imaging in renal trauma, S Gamanagatti, 2013
When Is Surgery Required Versus Conservative Management?
Surgical or interventional radiology procedures are indicated when the patient is hemodynamically unstable, shows ongoing hemorrhage, or when imaging reveals expanding hematoma or vascular injury. Conversely, stable patients with low-grade injuries (small lacerations or contusions) are managed conservatively with observation, restricted activity, and serial imaging or labs. Interventional embolization offers a minimally invasive alternative to open surgery for controlling bleeding in select cases; open repair is reserved for complex injuries or failed embolization. Decisions depend on real-time hemodynamics, imaging findings, and the treating trauma team‘s judgment.
What Does Conservative Management Involve?
Conservative management centers on activity restriction, bed rest initially, and close monitoring with serial vital signs and hematocrits to detect delayed bleeding. Pain control is tailored to avoid masking worsening symptoms while supporting mobility; anti-inflammatory and opioid-sparing measures are preferred when appropriate. Imaging follow-up—often repeat ultrasound or CT at scheduled intervals—confirms hematoma stability and healing progression. Structured clearance protocols progressively reintroduce aerobic conditioning, core strengthening, and supervised sport-specific drills only after clinical and imaging benchmarks are met.
What Is the Typical Recovery Timeline for Football Players with Kidney Injuries?
Recovery timelines vary by injury grade, patient age, and treatment approach, but clinicians use staged milestones to plan return-to-play. Minor contusions and low-grade lacerations often permit return to non-contact activity in 2–6 weeks, while severe lacerations that required embolization or surgery can require many months of graded rehabilitation and extended renal monitoring. Rehabilitation emphasizes a phased increase in aerobic activity, progressive core and trunk conditioning to protect the flank, and careful staged exposure to contact drills. The table below maps injury severity to typical recovery ranges and RTP milestones to set realistic expectations for athletes, families, and coaching staff.
How Long Does Recovery Take for Minor to Moderate Kidney Injuries?
For minor to moderate injuries, many athletes progress from initial rest to light aerobic exercise within 2–6 weeks, provided symptoms resolve and laboratory markers normalize. Progression follows a staged protocol: rest and monitoring → light cardio and core stability → non-contact sport-specific drills → controlled contact practice. Each step requires physician or athletic-trainer sign-off, with repeat imaging only as indicated by symptoms or clinical concern. This phased approach reduces re-injury risk and ensures the kidney has adequate time to resolve hematoma and parenchymal inflammation before contact is resumed.
What Are the Recovery Expectations for Severe Kidney Lacerations?
Severe lacerations often necessitate prolonged recovery, with some athletes facing several months before full contact return and ongoing monitoring for late complications like hypertension or reduced renal function. After surgical repair or embolization, initial in-hospital recovery is followed by staged outpatient rehabilitation and periodic renal function testing. Rehabilitation emphasizes gradual cardiovascular conditioning and progressive trunk strengthening while avoiding contact until imaging confirms structural stability. Realistic timelines require coordination among sports physicians, urologists, and athletic trainers to balance competitive goals with long-term renal health.
What Physical Therapy and Rehabilitation Are Recommended?
Rehabilitation focuses on progressive aerobic conditioning, core and oblique strengthening to protect the flank, and functional movement retraining that reduces torque on the abdomen. Physical therapists and athletic trainers design programs that begin with low-impact cardio and isometric core work, advancing to rotational drills and plyometrics only after tolerance is confirmed. Sport-specific conditioning reintroduces cutting, tackling technique modifications, and supervised contact simulations under medical clearance. This staged plan enhances physical readiness while directly addressing biomechanical risk factors that contributed to the original injury.
How Does Mental Health Impact Athlete Recovery?
Psychological response to significant injury—including anxiety about recovery, fear of re-injury, and social isolation during rehabilitation—can slow adherence and impair performance when returning to play. Integrating mental–health support, such as sports psychology sessions, peer support from teammates, and clear communication from coaches, improves motivation and recovery outcomes. Cognitive strategies and graded exposure to sport-specific stressors help athletes rebuild confidence before full contact return. Addressing mental health is therefore integral to the physical rehabilitation plan, not an optional add-on.
When Can Football Players Safely Return to Play After a Kidney Injury?
Safe return-to-play (RTP) requires a combination of objective medical clearance, symptom resolution, and staged exertion testing under supervision. Medical benchmarks include normalized labs (no persistent hematuria, stable hemoglobin), imaging confirmation of resolving hematoma or repair integrity, and specialist clearance from a sports physician or urologist. Functional milestones include completion of graded aerobic capacity tests and successful non-contact to contact progression supervised by athletic training staff. The checklist below summarizes the essential criteria clinicians use before allowing return to full contact competition.
- Medical Clearance: Signed approval from a sports medicine physician or urologist after review of labs and imaging.
- Symptom Resolution: No flank pain, no hematuria, and stable vital signs at rest and on exertion.
- Functional Testing: Successful graded exertion tests and completion of non-contact drills without pain.
- Imaging/Lab Benchmarks: Repeat imaging or labs as indicated to confirm structural healing and stable renal function.
What Medical Clearance Is Needed Before Returning to Football?
Clearance typically requires evaluation by a sports medicine physician, often with consultation from a urologist for higher-grade injuries, plus objective testing including creatinine/urinalysis and, where indicated, follow-up imaging. The clearing clinician confirms that renal function is stable, there is no ongoing bleeding, and the athlete tolerates graded exertion without symptoms. Clearance should also document a plan for progressive reintroduction of contact and specify monitoring frequency for the first season back. This multidisciplinary clearance process minimizes the likelihood of re-injury and long-term renal sequelae.
What Symptoms Must Fully Resolve Before Resuming Contact Sports?
Athletes must be free of flank or abdominal pain, have no hematuria on urinalysis, maintain stable vital signs, and show normal or baseline renal function on laboratory testing before resuming contact. Persistent pain or any evidence of ongoing bleeding mandates further evaluation and postponement of contact activities. Absence of symptoms during progressive exertion and contact simulations is a practical test of readiness and must be documented before clearance. These symptom-based thresholds protect both immediate safety and long-term renal outcomes.
How Do Doctors Monitor Long-Term Kidney Health Post-Injury?
Long-term monitoring includes periodic checks of renal function (serum creatinine, estimated GFR), blood pressure surveillance, and repeat imaging if clinical findings suggest delayed complications. Monitoring intervals vary by injury severity—from a few weeks for minor injuries to annual follow-up after severe lacerations—and aim to detect hypertension, reduced renal reserve, or scarring. Early detection of late sequelae enables timely interventions that preserve long-term kidney health, so coordinated follow-up with primary care and specialist teams is vital.
How Can Kidney Injuries Be Prevented in Contact Sports Like Football?
Prevention combines protective equipment, coaching technique, conditioning, and education on early symptom reporting to reduce incidence and severity of renal trauma. Properly fitted flank guards and chest protectors can dissipate force away from the kidney-bearing region, while tackling mechanics that emphasize shoulder contact and safe body position reduce direct blows to the flank. Conditioning programs that enhance core strength and flexibility help athletes tolerate impacts more safely. The table below compares common protective measures, how they help, and their practical limitations.
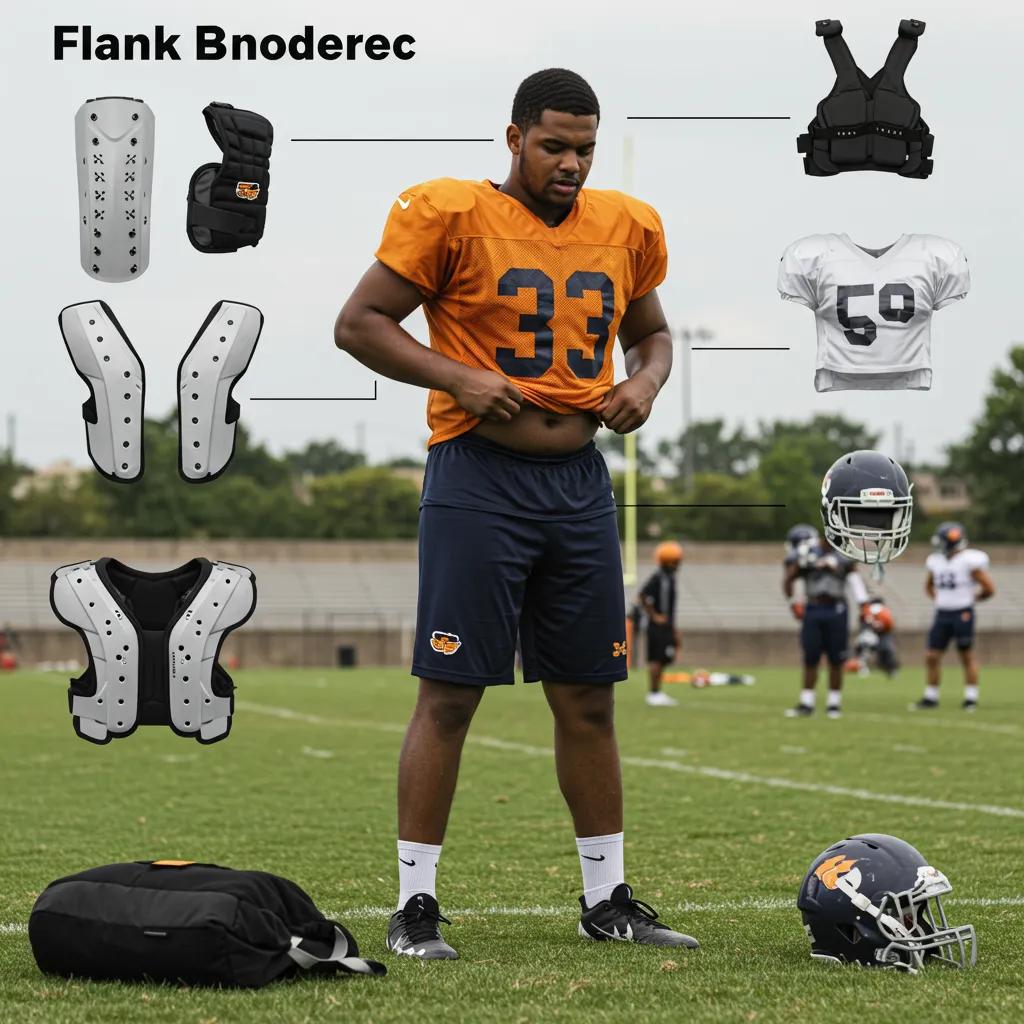
What Protective Equipment Helps Reduce Renal Trauma?
Flank-specific padding and well-designed chest protectors reduce localized force transmission to the kidneys by spreading the impact across a wider surface. Proper helmet and shoulder-pad fit also influence the mechanics of collisions, indirectly reducing risky flank exposures. However, no padding eliminates all risk; comfort, fit, and athlete compliance are crucial for effectiveness. Teams should balance protection with mobility and coach education on consistent use during practices and games.
How Does Proper Technique Lower Injury Risk?
Technique adjustments—such as emphasizing shoulder-led tackles and reducing head-down or side-impact approaches—direct force away from the torso and reduce flank impacts that can injure internal organs. Coaches can integrate drill progressions that reward body positioning, hip control, and wrap mechanics to create safer habits. Strength and flexibility work targeting the trunk and obliques further protect the torso by increasing energy absorption during collisions. Technique combined with conditioning produces sustained reductions in internal-organ injury risk.
What Role Does Athlete Awareness Play in Prevention?
Athlete education about recognizing hematuria, flank pain, or lightheadedness after a hit encourages early reporting and rapid evaluation, reducing delays that worsen outcomes. Creating a culture where players feel comfortable reporting symptoms without stigma is essential for timely care. Teams that implement pre-season education, sideline symptom checklists, and straightforward reporting protocols see faster triage and fewer delayed complications. Early reporting links prevention directly to improved diagnostic and treatment outcomes.
What Is the Latest Update on Justin Landes’s Recovery and Community Support?
Local coverage indicates Justin is in recovery and receiving follow-up care while the Lake High School community organizes support for the player and family. Reports emphasize that his immediate medical needs were addressed promptly, and the focus now is on staged rehabilitation and monitoring for full renal recovery. Community response—from teammate support to school announcements—has centered on practical assistance and morale, reinforcing how local networks mobilize after high-school sports injuries. ARY News will continue to track verified updates as they become available and summarize expert guidance for readers following his progress.
Within ongoing coverage, ARY News is continuing to report verified updates and will publish follow-up details as clinicians and the family provide them. For readers tracking this story, ARY News’s role as an information hub focuses on timely, factual updates and context about the medical and athletic steps ahead. This brief update reflects the editorial intent to provide timely and comprehensive news and current affairs coverage, keeping the audience informed and engaged with diverse content. The next subsections outline probable medical progress milestones, community actions commonly observed in similar cases, and expert perspectives on prognosis and return-to-play expectations.
How Is Justin Landes Progressing After Surgery and Treatment?
Available reports indicate he is progressing through early recovery phases with medical supervision; clinicians typically monitor pain control, mobility, and laboratory markers as immediate recovery markers. Early milestones commonly include transition from inpatient observation to outpatient rehabilitation once hemodynamics and labs stabilize, followed by graded activity progression in coordination with athletic trainers. Pain levels and mobility guide the pace of physical therapy, while repeat imaging or labs confirm structural healing. These objective measures determine when staged exertion and sport-specific conditioning can safely begin.
What Support Has the Cleveland and Lake High School Community Provided?
Communities often respond with tangible support: organized meal trains, fundraising for medical expenses, attendance at team events to show solidarity, and school-led communications offering updates and resources to families. Teammates frequently dedicate games or wear support gear, while boosters and alumni coordinate fundraising or volunteer assistance. Such community actions contribute to emotional recovery and practical needs during prolonged rehabilitation. These community responses also reinforce safety culture by spotlighting the importance of medical care and institutional support for injured athletes.
What Insights Do Sports Medicine Experts Offer on His Recovery?
Sports medicine experts emphasize that prognosis depends on initial injury grade, hemodynamic stability, and timely intervention, with most low- to moderate-grade injuries achieving full recovery when managed appropriately. Specialists recommend multidisciplinary follow-up—including sports physicians, urologists, and athletic trainers—and stress that return-to-play decisions should be milestone-based rather than purely time-based. Emerging rehabilitation trends through 2025 emphasize integrated physical and mental–health support, targeted core strengthening, and individualized RTP protocols to optimize long-term function and athlete confidence.
For continuing updates on this case and related local sports safety reporting, follow ongoing coverage on the ARY News Sports page.
Conclusion
Understanding kidney injuries in football is crucial for ensuring athlete safety and effective recovery. By recognizing symptoms, implementing preventive measures, and following structured rehabilitation protocols, players can return to the field with confidence. Stay informed about the latest updates and expert insights to support injured athletes in your community. For more resources on sports safety and recovery, explore our comprehensive articles today.